Enamel Defects
Dental Specialists caring for children’s oral health
Enamel defects are common in children. Enamel makes up the outer layer of the tooth and performs an important role in providing strength during function, protection from dental caries (decay) and gives the white appearance to the tooth.
Enamel defects can reduce the strength of the tooth, increase the risk for dental caries and cause cosmetic concerns, amongst many other issues. They can increase the need for dental treatment from a young age and throughout life.

The most common enamel defects affect the first permanent molars. Management of the defective first permanent molar present the greatest challenges to patients and their dental practitioners and this information guide will focus mainly on Molar Hypomineralisation (MH).
The AAPD would like to thank and acknowledge Dr Rebecca Williams (Perth) and her colleagues in the development of these valuable resources.
Defects in the enamel occur during amelogenesis (enamel development) whilst the tooth is still under the gingiva (gums), before erupting into the mouth. The stage at which enamel development is affected and the age at which the disruption/damage occurs will determine the type of defect and which teeth are involved. Enamel defects can affect both the primary and permanent teeth and in most cases are not preventable.
Other forms of enamel defect such as dental fluorosis, enamel hypoplasia (Chronological Enamel Hypoplasia and Turner Teeth) and Amelogenesis Imperfecta also exist, having separate and distinct clinical features, considerations and aetiological factors.
Primary Teeth
|
Tooth |
Tooth development begins (initiation) (weeks in utero) |
Calcification of enamel begins (weeks in utero) |
Crown completion (months) |
|---|---|---|---|
|
Central incisor |
7 |
13-16 |
1-3 |
|
Lateral incisor |
7 |
14-16 |
2-3 |
|
Canine |
7.5 |
15-18 |
9 |
|
First molar |
8 |
14.5-17 |
6 |
|
Second molar |
10 |
16-23.5 |
10-12 |
Permanent Teeth
|
Tooth |
Tooth development begins (initiation) (months in utero) |
Calcification of enamel begins |
Crown completion (years) |
|---|---|---|---|
|
Central incisor |
5-5.25 miu |
3-4 months |
4-5 |
|
Lateral incisor |
5-5.25 miu |
3-4 months |
4-5 |
|
Canine |
5.5-6 miu |
4-5 months |
6-7 |
|
First premolar |
Birth |
1.75-2 years |
5-6 |
|
Second premolar |
7.5-8 months |
2.25-2.5 years |
6-7 |
|
First molar |
3.5-4 miu |
Birth |
2.5-3 |
|
Second molar |
8.5-9 months |
2.5-3 years |
7-8 |
|
Third molar |
3.5-4 years |
8-10 years |
12-16 |
Cameron, A. & Widmer, R. (2008) Handbook of Pediatric Dentistry, 3rd ed., Sydney: Elsevier.
Molar Incisor Hypomineralisation (MIH) is a condition characterised by distinctive enamel opacities (patches of colour), typically affecting one to four first permanent molars, with or without incisor involvement. Hypomineralised enamel has less mineral and higher protein than normal enamel, which weakens the tooth. Affected molars present physical challenges and are prone to rapid breakdown, sensitivity and dental caries, whilst incisors are more likely to present concerns about appearance. Other teeth commonly affected by hypomineralisation include the second primary molars and occasionally permanent canines.
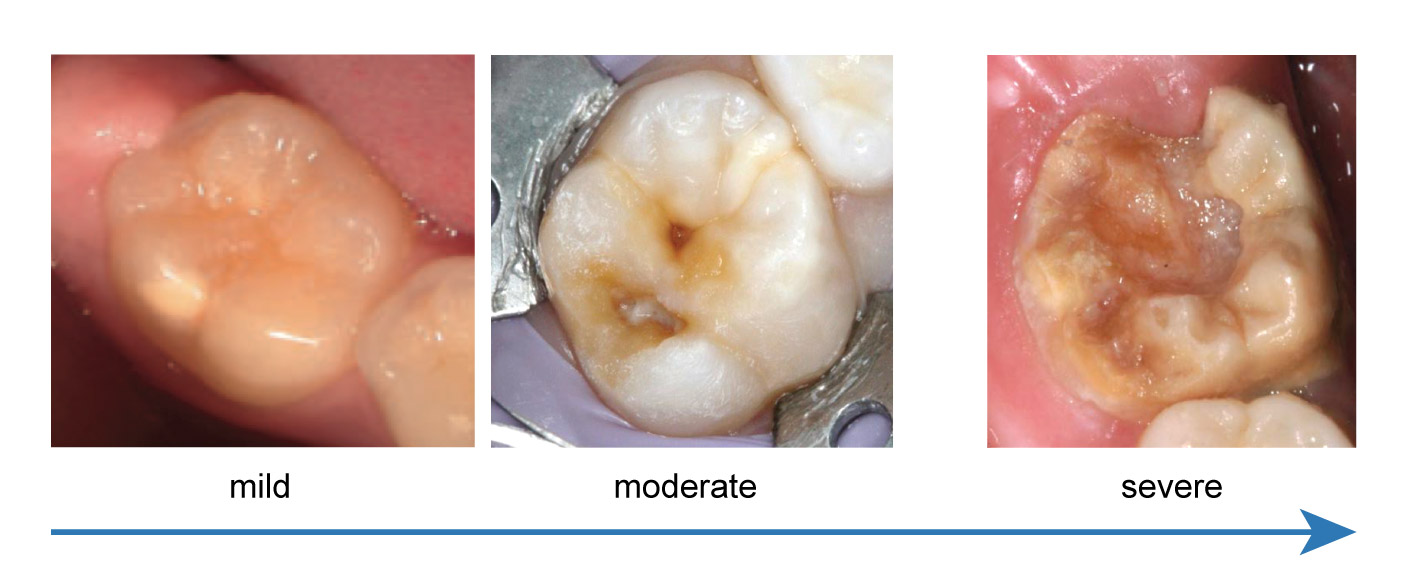
- Distinct patches of colour on the tooth which may vary from white, yellow, orange to brown.
- The number of teeth affected may range from 1-4 first permanent molars and the severity between these teeth may also vary from mild, moderate to severe. Incisors may or may not be affected.
- The affected enamel is of normal thickness but is weak.
- Sensitivity to temperature and touch is common.
- Breakdown and dental caries is very common.
- Dental caries and restorations (fillings) can be of an unusual shape and size.
Molar Hypomineralisation affects approximately 1 in 6 Australians (16%). Males and females are affected equally.
The cause of MH is not known and the condition is not preventable at this time. There is a disruption in the enamel maturation process occurring between late pregnancy and the first three years of life. There is considerable evidence for an association between early childhood illness and MH, however it is likely that multiple factors are at play with possible genetic, environmental and post-maturation influences.
There is no universal classification for MH, however severity is generally determined by the colour, location, presence of the enamel breakdown and sensitivity.
Suspicion for MH should be heightened for children who have had early childhood illnesses or hypomineralised second primary molars. Scheduling dental appointments to ensure the first permanent molars are assessed shortly after eruption is ideal. The average age for eruption of the first permanent molar is six years of age.

- Reduced physical properties (weak enamel).
- Increased dental caries.
- Increased sensitivity to temperature and touch.
- Reduced effectiveness of local anaesthesia.
- Decreased restoration longevity (repairs do not last as long).
- Increased dental treatment required.
- Increased dental fear and anxiety, likely due to increased dental treatment from a young age and sensitivity/difficulty to anaesthetise (numb).
Hypomineralised teeth are at an increased risk of dental caries and sensitivity. Adult strength (1200-1450ppm) fluoridated toothpaste with supervised brushing twice daily is recommended. Placement of fissure sealants where hypomineralisation defects are present on the occlusal (biting) surface can be beneficial. Topical fluoride varnishes, desensitizing toothpastes and remineralising agents (e.g. CPP-ACP) may be an additional adjunct in reducing caries risk and hypersensitivity. Resin infiltration to strengthen hypomineralised enamel is a promising area of research. The dental health professional will tailor a preventive approach suitable for the individual tooth.

Where there is enamel breakdown or dental caries, the restoration of choice will depend on the size of the lesion and surfaces affected. Composite restorations (white fillings) are the material of choice for smaller lesions. Bonding of the restoration to hypomineralised enamel is inferior to that of normal enamel, and so may need replacing more frequently. If the lesion is particularly large and/or involving the cusps, a stainless steel crown (capping) is usually required.

Hypersensitivity and reduced effectiveness of local anaesthetics means that sedation is often required for dental treatment of affected molars. Patients may also have heightened fear and anxiety due to increased treatment needs at a young age. Nitrous oxide sedation, also known as “happy gas” or general anaesthesia is often required for successful management.
Extraction of compromised teeth is an acceptable and important consideration – particularly where there is infection, toothache, where multiple surfaces of the tooth are broken down or there is insufficient tooth structure remaining to maintain. When considering the extraction of a first permanent molar, the ideal timing, presence of permanent third molars (wisdom teeth), existing occlusion (bite) and need for additional extractions should be assessed. An orthodontic opinion is highly recommended so that a multi-disciplinary management plan can be better formulated and discussed with appropriate consent.
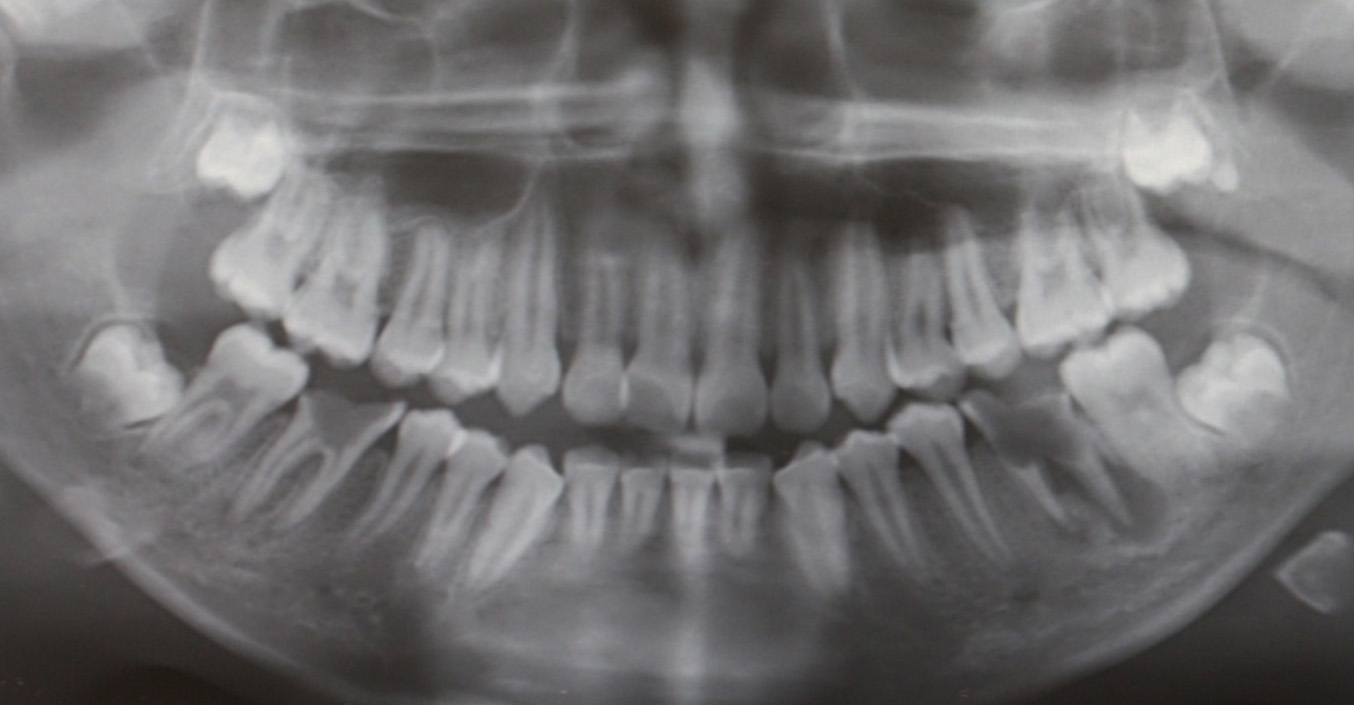

A radiograph and clinical photograph of severe MH with post-eruptive breakdown, dental caries and pulpal (nerve) infection. Extraction is indicated.
Other Types of Enamel Defects
Dental fluorosis is a defect of enamel resulting from a high intake of fluoride while the teeth are developing. The severity of fluorosis is dependent on the dose, timing and duration of excessive fluoride exposure.
Milder cases present as diffuse, generalised white flecking defects or horizontal narrow banding across the enamel. Severe cases may be yellow to dark brown with pitting (stain and breakdown occurring following eruption).
Fluorosis is symmetrical between the same teeth on either side of the mouth. In Australia, cases of fluorosis are typically very mild to mild, with severe cases being very rare.

A mild case of dental fluorosis affecting the permanent maxillary central incisors – white flecking of the enamel is noted.
Dental fluorosis was first identified in communities where the natural fluoride concentration in drinking water was very high (far exceeding the levels used in community water fluoridation). Those with fluorosis were also noted to have reduced rates of dental decay.
Community water fluoridation has been a very successful public health measure in reducing dental caries levels across the population. Optimal water fluoridation levels are considered to be 0.6 – 1.1ppm fluoride for maximum caries prevention effects whilst minimising dental fluorosis.
Individual variation in fluorosis for the same water fluoride intake occurs between and within populations. Factors that may affect susceptibility to fluorosis include dietary fluoride sources, environmental fluoride and individual physiological factors.
The main concern in relation to dental fluorosis is the appearance of affected incisors. Depending on the extent of fluorosis and age of the patient, treatment options include microabrasion, tooth whitening, veneers (composite or porcelain) or a combination of these techniques. In children, a cautious approach should be taken and the most conservative treatments attempted first.
Enamel hypoplasia is an enamel defect which results in thinner enamel of normal strength and physical properties. It may affect all teeth undergoing enamel development at the same time, known as chronological enamel hypoplasia, or only one tooth where a localised disturbance has occurred during development. Localised disturbances include dental trauma or infection to the primary tooth above where the permanent tooth is developing. The permanent incisors are most at risk of trauma-related hypoplasia, whilst the permanent premolars are most at risk of infection-related hypoplasia due to increased incidence of caries and infection in the primary molars.

The main clinical considerations relate to an increased risk of decay due to difficulty in maintaining oral hygiene in areas of hypoplasia which allows plaque to collect. Another significant issue is in relation to appearance and cosmetic concerns.
When plaque retention or aesthetics are of concern, a restoration (filling, veneer or crown) may be placed over the hypoplastic area to make the tooth more uniform in appearance and easier to brush. As the enamel is of normal quality, the restoration will bond to the tooth with similar strength as in unaffected cases. In children, an interim direct restoration (white filling or composite veneer) may be the most appropriate option until growth completion – when porcelain veneers, ceramics and crowns may be considered.
Amelogenesis imperfecta (AI) is a group of rare, inherited enamel defects. The defects characteristically affect all of the primary and permanent teeth and vary in appearance depending on the gene that is defective and the phase of enamel development that the gene controls. Heredity may be X-linked, autosomal dominant, autosomal recessive or spontaneous mutations. In most cases, there is a known family history of the condition.
There are multiple forms of AI, grouped into several types – Hypoplastic AI, Hypomaturation AI, Hypocalcification AI, Hypoplastic-Hypomaturation AI with Taurodontism.

Dental management varies markedly across different cases of AI as presentation and severity of the condition is highly variable. In general, definitive aesthetic dental treatment for children should be delayed as long as possible to allow the tooth to develop, the pulp to recede and the gingiva to mature and maintain its level. In AI however, social issues related to the appearance of the teeth tend to occur early and a transition phase of restorative care is often necessary soon after the teeth erupt.
The main clinical concerns relate to aesthetics and associated hypersensitivity (and difficulty with chewing), with an increased risk for dental caries and tooth wear. High levels of patient cooperation over multiple visits are required for management which can be challenging for children.
Links to other dental conditions such as abnormal development of the pulp chamber (taurodontism), eruption delay or failure, anterior open bite, missing teeth, crown and/or root resorption, hypercementosis and pulpal calcifications can also be found. Links to medical conditions such as nephrocalcinosis has also been noted, with recommendation for renal examination at time of AI diagnosis.
Aggressive preventive protocols should be introduced following diagnosis of AI. Good oral hygiene, fluoride toothpaste and remineralisation paste (e.g. CPP-ACP) should be utilised to reduce risk of caries, sensitivity and tooth wear. Microabrasion and tooth whitening are a good starting point for improving the appearance of AI, however tooth whitening may cause temporary sensitivity in some cases.
Composite restorations can be used where enamel breakdown or caries is minimal. These are challenging due to reduced bond strengths to the abnormal enamel. Onlays can be considered if there is sufficient enamel to bond to, as they are more conservative than crowns.
Stainless steel crowns are often used where there is marked breakdown of the teeth. These cover the teeth completely to protect them until growth completion when they can be replaced with a permanent crown.
Composite veneers, with a view for replacement with porcelain crowns and ceramics after completion of growth, may be required soon after eruption in more severe cases. Depending on the original colour of the teeth, masking of the underlying defect may be difficult, however there are opaquing materials available which assist with this.
For more information on Developmental Dental Defects, please go to www.thed3group.org